Cure Idiopathic Pulmonary Fibrosis
Treatments
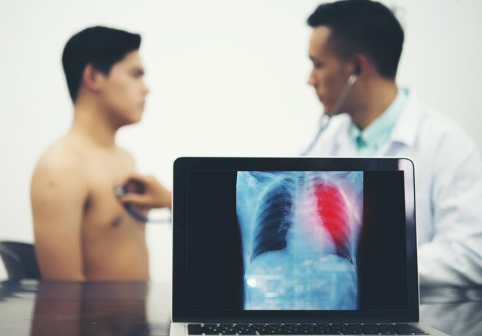
Idiopathic pulmonary fibrosis (IPF) is a dangerous lung disease that affects breathing and the way of life. It complicates the entry of oxygen into the blood mass by scalding and hardening the lungs. This scarring becomes more severe with age leading to exhaustion, shortness of breath and reduced quality of life. Although there is no permanent cure, considerable progress in the treatment of IPF has been achieved by the way of drugs, therapies and lifestyle change. To provide the patients with hope and a means of coping with the disease, this paper analyses the possible treatments, studies and viable solutions.

Understanding Idiopathic Pulmonary Fibrosis
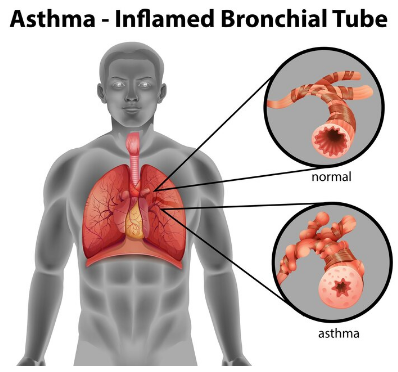
Global scarring of the lungs of unknown cause is referred to as idiopathic pulmonary fibrosis (idiopathic means unknown cause). This process of the thickening of the lung tissue and its hardening due to the formation of scar tissue is known as fibrosis. This scarring gradually decreases the ability of the lungs to expand and efficiently exchange oxygen.
The symptoms of IPF, including constant dry cough, dyspnea in general movement, and recurring fatigue, can often develop gradually. As the illness progresses, patients can also develop dyspnea when they are resting. Even though it is not clear what exactly causes the disease, aging, exposure to the environment (smoke or dust), and genetic factors are also involved in the disease.
Is There a Cure for Idiopathic Pulmonary Fibrosis?
At the moment, idiopathic pulmonary fibrosis is still incurable. The scarring of the lung that has already been acquired cannot be reversed. Nevertheless, effective therapies can be found in contemporary medicine that can reduce the symptoms, decelerate the process, and significantly raise the quality of life and longevity.
Treatment of IPF is done to stop further destruction of the lungs, reduce the difficulty of breathing, and to ensure that all-over health is improved. When properly cared for, treated, and able to effectively get emotional and psychological support, a great number of IPF patients can enjoy active and satisfying lives over several years.

Medications That Slow the Progression of IPF
Two significant medications have altered the treatment of IPF:
Esbriet (pirfenidone)
Antifibrotic medication known as pirfenidone helps to reduce the amount of scar tissue in lungs. It is able to elevate the survival rates and delay the decline of the lung functioning. This is an oral drug that is usually prescribed to patients with mild to moderate IPF.
Patients may have mild side effects, such as nausea or skin sensitivity, but they can be treated through regular check-ups and drug adjustments. Pirfenidone retards the escalation of the symptoms and stabilizes breathing.
(Ofev) Nintedanib
Nintedanib works in a different way by inhibiting several growth factors resulting in scarring of the lungs. It also reduces the pace by which the lung functioning degrades, and thus the patients will be able to breathe more comfortably over the long run.
The drug is administered twice a day and should be used with food and is applicable at the majority of IPF stages. The most common side effects include diarrhea and stomach discomfort which can through supportive measures be generally controlled. Pirfenidone and nintedanib have both demonstrated effectiveness as symptom-controlling and life-prolonging drugs.
Lung Transplantation: The Only Potential Cure
The idiopathic pulmonary fibrosis has only known treatment which is a lung transplant although the drugs can slow the condition. It is a process that involves the replacement of the damaged lungs by healthy ones donated by another individual, and the process enables normal breathing to resume.
In other healthy patients who are less than 70 years old and fit some standards, lung transplantation is normally recommended. Despite the hope that the surgery offers a new life, there are disadvantages such as long waiting lists, the post-surgery risks, and the need to take a life long medication so as to avoid rejection.
These challenges notwithstanding, transplant success rates are on the increase and the recipients are living happy and full lives.
Oxygen Therapy: A Lifeline for Easier Breathing
The blood oxygen level is decreased as IPF progresses and causes exhaustion and dyspnea. Oxygen therapy is important at this stage. It ensures that the body receives sufficient oxygen to operate well by supplying inadequate oxygen.
Oxygen can be administered on a continuous basis depending on the condition of the patient or just on a need-to-need basis when the patient is on the move. Portable oxygen concentrators help in making it easier to maintain an active lifestyle and social life. Besides making people more comfortable, oxygen therapy reduces the load on the heart and prevents the development of complications.
Pulmonary Rehabilitation: Building Strength and Confidence
Pulmonary rehabilitation is a structured program that aims to be used in patients who have long-term lung diseases such as IPF. It includes emotional assistance, physical exercise, diet, and breathing exercises.
The patients who take part in these programs are informed on how to manage their symptoms, conserve energy, and breathe properly. Exercising helps in enhancing the muscles of the respiratory system making it easy to perform daily activities. More importantly, rehabilitation programs provide patients with encouragement and support of the community to them, making them feel less isolated in the process.
Lifestyle Changes That Support Lung Health
Even slight daily changes can make a big difference to the sufferers of IPF. Social factors include quitting smoking, preventing pollution, and physical activity to slow down diseases. Antioxidants, lean meats, and high in fruits increase the immune system and reduce inflammation.
Moreover, the infections may quickly worsen the functioning of the lungs, so the patients must receive their vaccinations against pneumonia and flu. Stress management can be improved through techniques such as meditation or therapy to improve breathing control and mental health.
Managing Cough and Breathlessness
One of the most disturbing symptoms of IPF is breathlessness and chronic cough. A few tactics can be useful:
Breathing techniques: Breathlessness can be reduced through the application of diaphragmatic and pursed-lip breathing.
Drug: Opioid analgesics, cough suppressants, and anti-reflux drugs can be used to relieve pain.
Positioning: Sitting straight or bending slightly forward may help in making breathing easier.
Humidifiers: The air in the home needs additional water, which will prevent the development of cough and ease the throat.
These symptoms can be effectively managed through a combination of medical care and reasonable lifestyle modification interventions in the patients.
Emerging Research: Hope for the Future
People everywhere are busting their brains trying to crack idiopathic pulmonary fibrosis—basically, finding a way to actually fix the lungs instead of just putting a band-aid on the problem. And honestly? There’s some wild stuff happening in labs right now.
Take stem cell therapy. Scientists are poking around to see if these little miracle workers can patch up busted lung tissue. If they pull it off, that’s some sci-fi level healing right there.
Gene therapy’s another hot topic. Some folks get IPF because of genetic glitches—so the idea is, fix the code, stop the damage. Easier said than done, sure, but the logic’s there.
Then there’s the anti-inflammatory and antioxidant crew. They’re basically fighting the lung fire—trying to chill out the inflammation that makes things worse.
And get this: researchers are building these teeny-tiny nano-drug carriers (think: microscopic delivery trucks) to haul meds right to the damaged lung cells. No more hoping the drugs wander to the right spot—they’ll just get an express delivery.
Bottom line, none of these are ready for prime time yet. But, man, the hope’s real. Maybe in the not-so-distant future, we’ll actually have something that cures this mess for good. Wouldn’t that be something?
The Role of Nutrition in Managing IPF
Honestly, if you want your lungs working at full blast, you gotta pay attention to what you shovel into your mouth. Don’t overthink it—aim for stuff that’s not gonna drag you down: whole grains, some lean chicken or fish, a rainbow of fruits and veggies. Those things are basically your body’s pit crew.
Oh, and if you can pack in foods loaded with antioxidants, omega-3s, and vitamin C? That’s like giving your insides a spa day. They help keep inflammation from turning your lungs into a drama zone. On the flip side, salty junk or anything processed? Yeah, those will just make you puffy and miserable. Heavy meals, too—skip ‘em unless you want to feel like you’re trying to breathe through a straw.
One more thing: stay hydrated. Seriously. Water keeps your mucus from turning into cement, so breathing isn’t a chore. Simple as that.
Emotional Health and IPF: Coping with the Diagnosis
Getting hit with an IPF diagnosis? Yeah, that can totally knock the wind outta you. Fear, anxiety, just not knowing what’s next—it’s all pretty normal. Honestly, having someone to lean on makes a world of difference. I mean, nobody should have to tough it out alone.
Support groups? Those are gold. You get to swap stories, maybe even pick up a few tricks for handling the rough days. Mindfulness stuff and talking to a counselor—hey, it’s not all “woo-woo;” it can actually chill you out and help you see a little light at the end of the tunnel. And let’s not forget family and friends—they’re the real MVPs. Whether it’s a shoulder to cry on or someone to bring you snacks, they’re right there in the trenches with you.
Preventing Complications in IPF
Honestly, with IPF, your lungs are kind of running on low battery all the time, which makes picking up infections way too easy. So, what do you do? First off, get those flu and pneumonia shots—just do it, no excuses. You don’t want to end up in the hospital over something you could’ve dodged.
If someone’s coughing up a storm? Nope, don’t go near them. Not worth the risk. And if you’ve gotta be somewhere sketchy, like a crowded subway or a place with gross air, throw on a mask. Wash your hands like you’re about to perform surgery (okay, maybe not that intense, but you get the idea).
Oh, and your heart’s working overtime when your lungs aren’t pulling their weight, so keep an eye on that. Eat some veggies, move around, don’t ignore chest pain. Seriously.
Pop by your doctor’s office on the regular too—don’t just wait for things to get bad. They’ll keep tabs on your lungs and catch problems early.
All this stuff? It’s annoying, sure, but it actually helps you feel better and puts the brakes on the disease a bit. Quality of life > complications, every time.
Complementary and Alternative Therapies
Besides regular therapy, a lotta folks go hunting for alternative stuff. It can totally boost your overall care—just don’t go ditching your meds for a yoga mat, alright? Things like yoga, acupuncture, or popping some herbal supplements might chill you out, help you breathe easier, make you feel kinda zen. But, listen, some herbs seriously mess with IPF meds, so don’t play doctor. Run it by your actual doctor first before you start experimenting.
Living with IPF: Staying Active and Hopeful
Honestly, living with idiopathic pulmonary fibrosis isn’t exactly a walk in the park, but you know what? A ton of folks still find ways to enjoy life. Staying active helps, sure, but don’t underestimate the power of hanging out with good friends or just setting some goals that actually make sense for your life right now—none of those pie-in-the-sky resolutions.
Medicine’s come a long way, too. Between new treatments, oxygen tanks that don’t make you look like a robot, and some pretty solid rehab programs, people are still out here traveling, picking up new hobbies, and spending real time with family. It’s not about just scraping by or surviving—managing IPF is about squeezing the good out of every day, even if some days are a little rough around the edges.
The Importance of Regular Medical Follow-Up
Look, tracking IPF isn’t something you just tick off a list and forget about—nah, you gotta keep at it. And so do your docs. Pulmonologists? They’re basically like the mechanics for your lungs, busting out all their sci-fi gadgets—spirometry, high-def CT scans, the works. Always poking around, fiddling with your oxygen, switching up your meds, suggesting tweaks to your PT routine. It’s not some pointless red tape either. These check-ins? They’re the early warning system. Catch stuff before it blows up in your face. And honestly, if your healthcare squad actually listens and you don’t dread talking to them? That’s the real magic trick for not getting steamrolled by this disease over time.
Patient Support and Community Resources
Dealing with IPF? Yeah, it sucks, but you seriously don’t have to tough it out solo. There’s a ton of groups—think American Lung Association, Pulmonary Fibrosis Foundation, all those big names—that are way more helpful than just shoving leaflets in your face. They’ve got the goods: stuff like real-deal clinical trial info, support groups where you can actually talk to humans, counseling, you name it.
And, look, talking to people who actually get it? Total game-changer. Misery might not exactly love company, but hey, solidarity is pretty sweet. It’s just so much easier to keep your head up and not feel like you’re marooned somewhere when you know there are folks rooting for you. Plus, if you hang out in those online groups, you’re way more likely to catch the latest tips on lifestyle or new meds—basically, not get left in the dust.
Looking Ahead: A Future with Possibilities
IPF’s still got no cure, yeah, but honestly, research is picking up speed like it’s on a sugar rush. Scientists are out here saying new treatments might actually slam the brakes on fibrosis—or heck, maybe even back it up a bit. Wild, right? There’s a ton of buzz around personalized medicine too, where your DNA basically tells the doctors what to do next. Feels kind of sci-fi.
In the meantime, people aren’t just sitting around. Catch it early, get the right meds, maybe some oxygen, and tweak your lifestyle—suddenly you’ve got some control back. The outlook for folks with IPF? Not as grim as it used to be. Every year, there’s a little more reason to be optimistic. Hope’s not just a bumper sticker anymore.
Conclusion: Turning Hope into Healing
Look, idiopathic pulmonary fibrosis is a beast, and yeah—no magic cure yet. Still, hope isn’t dead. People are out here living their lives, and not just barely scraping by either. Oxygen tanks, those anti-fibrotic meds, rehab, just taking care of yourself—it all stacks up. Catching it early and actually sticking to the treatment plan? Huge. And honestly, having guts helps too.
Science isn’t sleeping on this. Every study, every new trial, it’s all slowly dragging us closer to something that might actually wipe out IPF for good. Until then, every little thing—whether it’s popping meds or just chilling with some deep breathing—makes a difference. It’s all about finding those small wins and not letting the disease call all the shots.
