Introduction and Overview Idiopathic
Pulmonary Fibrosis.
Idiopathic Pulmonary Fibrosis (IPF) is considered to be one of the most complicated and
destructive chronic lung diseases ever known to humankind. Idiopathic is a term that means the
cause is unknown and pulmonary fibrosis is a term that implies scarring and thickening of lung
tissue. This scarring is irreversible and extreme in the case of IPF which leads to stiffening of
the lungs and prevents them to supply the body with oxygen. Consequently, the patients are
affected with chronic dry cough, progressive shortness of breath, fatigue and decreased
exercise capacity.
IPF falls into the subcategory of interstitial lung diseases (ILDs) which involves diseases that
impact the tissue lining the alveoli – the small air sacs in which gases exchange. Though it is not
very common, its Geographic distribution of the world has risen in the last decades and
especially in males between the ages of 50 and 80 years. Average survival period after the
diagnosis is between three and five years, just like most types of cancer.
The characteristic of the IPF is the defective wound-healing process. In case the lung tissue is
damaged, rather than being repaired by normal means, the body forms too much of the fibrous
tissue, which leaves the lungs being scarred and less elastic. It is not known what causes this
disordered repair but a number of risk factors are identified. These are genetic mutations (in
genes, including MUC5B, TERT, and RTEL1), environmental toxins (e.g. metal dust or wood
smoke), tobacco use, viral infections, chronic acid reflux, which causes tissue damage in the
lungs over time.
Pathophysiology
In IPF, the abnormal cascade of cellular responses is caused by repetitive microscopic damage
of alveolar epithelium. The fibroblasts develop hyperactivity and release of collagen and
extracellular matrix proteins. This results in rigid scar tissue which replaces normal lung
parenchyma. All this leads to chronic hypoxemia due to a decrease in the diffusion of gases in
the alveolar walls. It is a silent process that takes years before one starts showing symptoms
and when that occurs, much damage has already been caused to the lungs.
Genetic Influences and Environmental Influences.
The genetic research indicates that there are some families that have a high tendency towards
IPF. Such a promoter variant as MUC5B raises the risk of the fibrosis occurrence, however,
could actually slow down the disease progression once it has developed. The process is further
accelerated by environmental triggers which include air pollution, farming dust, and viral
infections. Therefore, the emergence of IPF is a result of genetic predisposition and
environmental damage.
Clinical Presentation
The patients usually come out with slow onset of difficulty breathing and coughing with no
sputum. Lung-Auscultation- There is a crackling “Velcro-like sound. With the further progression
of fibrosis, digital clubbing (widening of the fingertips) and cyanosis (bluish color of the skin)appear. The symptoms, unfortunately, manifest themselves later, and it is the early diagnosis
that is important, by the time most of the lung tissue has scarred.
Current Treatment Options
Even after decades of research, no universal treatment of idiopathic pulmonary fibrosis has yet
been developed. Nevertheless, with the help of a number of treatments, it is possible to
considerably slow down its course and increase the quality of life.
Antifibrotic Medications
● Pirfenidone and Nintedanib have changed the management of IPF, as they have been
approved by the FDA.
● Pirfenidone (Esbriet) is both antifibrotic and anti-inflammatory. It inhibits the growth of
fibroblasts and the secretion of growth factors which stimulate scarring. Clinical trials like
CAPACITY and ASCEND have found out that Pirfenidone reduces the rate of lung
decline and can possibly prolong the life span slightly.
● Nintedanib (Ofev) is a tyrosine kinase inhibitor which inhibits several pathways –
platelet-derived, fibroblast, and vascular endothelial growth factor. The INPULSIS trials
have validated that Nintedanib decreases the yearly reduction in forced vital capacity
almost by half. The two drugs tend to be highly tolerated with the possibility of having
gastrointestinal side effects such as nausea or diarrhea.

Supportive and Symptomatic Care.
The IPF has an impact on breathing efficiency, which means that supportive care is crucial.
Additional oxygen therapy aids in the retention of oxygen and lessening of shortness of breath.
Pulmonary rehabilitation programs are programs of organized exercises under the supervision
of a doctor, which is beneficial to physical endurance and emotional wellbeing. Influenza and
pneumococcal infections have to be avoided by vaccinations in order to avoid complications.
There is also the importance of nutritional counseling, lifestyle changes, and psychological
assistance. IPF affects one in anxiety and depression and patient support group activities tend
to enable persons to manage the emotional load of having a chronic illness.
Lung Transplantation
Currently, IPF can be treated only through lung transplantation, which is likely to be cured. It
then replaces damaged lungs with fresh donor organs which provides a great deal of
prolongation of life and quality. The average life after the transplant is 5-7 years. Nevertheless,
all patients do not qualify because of age, comorbidities, or advanced disease at diagnosis.
There are still obstacles of donor shortages, surgical danger, and lifelong immunosuppression.
So, to the competent candidates transplantation is the nearest track towards a real cure.
New and Novel Therapies.
The cure is still sought, and advanced research has found some new measures, aimed at the
disease on a molecular level.
Gene and Cell-Based Therapy
● There is the study of genetic mutations that have crippled the ability of lung cells to
repair as therapeutic targets. One of the gene editing methods currently being examined
to repair mutations in TERT, TERC, or MUC5B is CRISPR-Cas9. Although still in early
stages of human trials, this research direction has the potential of preventing fibrosis at
its origin.● Another promising treatment is the stem cell therapy. Mesenchymal stem cells (MSCs)
that are produced by using either bone marrow or umbilical cord tissue exhibit the
potential to suppress inflammation, stimulate tissue healing, and control immune
reactions. Early clinical trials are positive in terms of safety and slight enhancement of
lung functioning, however, extensive research is required to prove their efficacy.

Novel Antifibrotic Agents
● In addition to Pirfenidone and Nintedanib, also other new medications are in clinical
trials:
● Pamrevlumab: a monoclonal antibody which targets connective tissue growth factor
(CTGF). Phase 3 trials indicate that it can slow the deterioration of the pulmonary
functions.
● PRM-151: a recombinant version of pentraxin-2 which regulates macrophages and
decreases fibrosis.
● BMS-986278: is an inhibitor of lysophosphatidic acid receptors which suppresses the
activation of fibroblasts.
➔ The combination therapy of these agents with current drugs could become a common
practice soon, in which various pathways of fibrosis are targeted simultaneously.
Regenerative & Tissue-Engineering Technology.
The technological development and progress of 3D bioprinting, as well as lung organoids,
enable researchers to create miniature lung tissue in the laboratory. These models are assisting
in determining the onset of fibrosis and how it can be reversed. The future of damaged lung
sections has been seen by researchers, in which bioengineered tissue patches could replace
the damaged parts.
Immunology Research and Microbiology Research.
● Recent research demonstrates that long-lasting immune activation and shifts in lung
microbiota is a factor leading to disease development. New treatment directions might be
provided by therapies aimed at the restoration of immune balance or altering the
microbiome.
● Current Research, Research Problems and Future Research Prospects.
Clinical Trials and Research.
● By 2025, tens of clinical trials are underway around the globe using new antifibrotic
drugs, gene therapies and stem cell therapies. Possible trials like the PRAISE
(Pamrevlumab) and ISABELA (GLPG1205) have given promising results. To detect
fibrosis earlier and monitor treatment discoveries, also advanced imaging techniques
and biomarkers are being developed.
Diagnosis and Prevention at an Early stage.
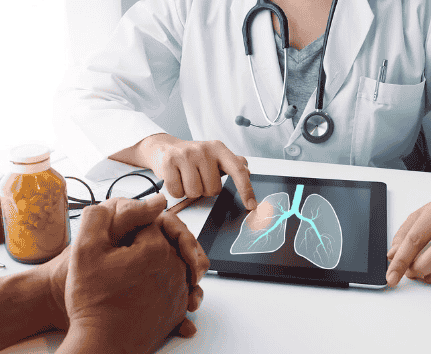
● The early detection is still important in enhancing the success. High resolution computer
tomography (HRCT) allows the radiologist to detect even the slightest fibrotic pattern
before the symptoms show up. Risk can be reduced with preventive measures such as
quitting smoking, limiting contact with industrial dusts and the treatment of acid reflux.
Genetic counseling can be used to assist families of inherited predisposition.
Palliative and End of Life Care.
● In more severe cases when the curative possibilities are no longer available, palliative
care guarantees comfort and dignity. Symptom management, psychological counseling,and home oxygen therapy increase the quality of life. Previous incorporation of palliative
care enables early planning of care by the patients and their families.
Barriers to a Cure
● The study of IPF is challenged by a number of issues:
● Complicated genetic, environmental and immune interactions.
● Diagnosis is made late when the scarring is permanent.
● Possesses low regenerative capability of lung tissue.
● Challenges in recruiting various patients into the long-term trials.
● All these obstacles are slackening the pace, yet international research cooperation is
slowly resolving them.
The Future of Hope
Over the past 10 years, IPF has become a discipline experiencing scientific breakthrough in
terms of its neglects. The antifibrotic medications have increased life span, transplantation has
actual survival advantages, and experimental therapy has potential regeneration instead of
mere control. Diagnosis and patient monitoring are also being transformed further using artificial
intelligence and digital health monitoring.
Although a full cure is yet to be made a reality, the intersection of genomics, regenerative
medicine, and precision therapy is becoming increasingly achievable. As the research continues
and the patients are also advocating, the dream of the curing of idiopathic pulmonary fibrosis,
which was thought to be impossible, is gradually becoming a medical fact.
