Pulmonary Fibrosis Oxygen Use
Pulmonary fibrosis is a progressive and chronic lung disease which makes breathing difficult. The ability of the lungs to supply oxygen to the bloodstream reduces as the lungs become scarred and hard. This has the effect of causing low oxygenation, fatigue, and persistent shortness of breath. One of the most effective approaches to the management of these symptoms and the improvement of the quality of life is oxygen therapy. We shall explore how the use of oxygen facilitates a healthier living, greater comfort and further activity of individuals with pulmonary fibrosis.

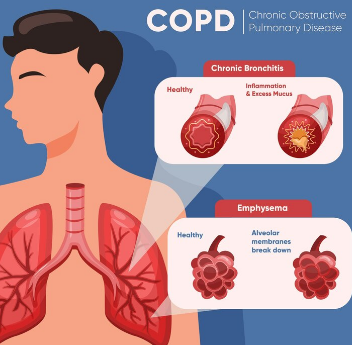
Understanding Pulmonary Fibrosis
When lung tissue thickens and scars, which is a phenomenon referred to as pulmonary fibrosis it makes it hard to get oxygen to the bloodstream. This scarring becomes increasingly more serious with time and breathing becomes extremely difficult. The disease can be caused by a plethora of reasons such as exposure to toxins, autoimmune diseases, infections, and unknown causes (idiopathic pulmonary fibrosis). The disease leads to a low oxygen saturation in patients, especially when the patient is in rest and most especially when the patient is exercising.
The main challenge regarding pulmonary fibrosis is that the scarring process cannot be undone but the symptoms may be managed. Oxygen therapy is required to provide relief of dyspnea, cardiac support, and overall body functions.
Why Oxygen Therapy Is Important in Pulmonary Fibrosis
The pulmonary fibrosis patients are unable to supply sufficient oxygen to the body due to the inadequacy of the lungs. Oxygen therapy fills this gap partly. It ensures that excess oxygen is supplied to body organs to enable them perform their functions well.
When the body lacks enough oxygen, it struggles to produce energy thus leading to fatigue, disorientation and a heart strain. Besides treating dyspnea and allowing the patient to perform daily tasks with less effort, oxygen therapy is also used to ensure that the level of oxygen saturation is kept normal (above 90). Moreover, it improves sleep, concentration, and overall mental health.
When Do You Need Oxygen for Pulmonary Fibrosis?
Doctors recommend oxygen therapy when the oxygen saturation of an individual drops below 88 percent when one is at rest or when one is exercising. This is normally measured using a pulse oximeter. Some individuals only require oxygen during the exercise and sleep time whereas others require it throughout the time of the day and night.
A low oxygen level is manifested by shortness of breath, bluish lips or fingertips, fatigue, lightheadedness, and rapid heartbeat. It is imperative to talk with your pulmonologist in case you experience the following symptoms. They will also conduct such tests as an arterial blood gas analysis or a six minutes walk test to determine whether you need oxygen therapy.
Types of Oxygen Therapy for Pulmonary Fibrosis
Oxygen may be administered in different forms in order to accommodate the needs of different individuals. Such systems as the most popular are:
Traditional metal vessels containing pressurized oxygen are known as compressed oxygen cylinders. They may be large and less portable although they are perfect at home.
Liquid oxygen systems are systems which store oxygen in liquid state and convert it to gas before inhalation. They are more portable and durable as opposed to compressed tanks.
Oxygen Concentrators: These are devices that provide continuous supply of oxygen by withdrawing it in the air. They are convenient and consume less energy to be used at home and on the move.
Each one is advantageous depending on the way of life, oxygen requirements, and physical activity. Your respiratory therapist and doctor will assist you to choose the most suitable system.
How to Use Oxygen Safely
Even though we need oxygen, its consumption should be in moderation. It is able to facilitate the heating of materials since it enhances combustion. Some basic precautions should therefore be taken by the user:
Store oxygen equipment outside the gas stove, candles and open flame.
In case of oxygen use, avoid smokers.
Cylinders must be stored erectly and in a cool and well ventilated place.
Check connections and Tubing- often check for leakages or damages.
Wear no petroleum-based products on your face like Vaseline when using oxygen.
These precautionary measures would help you to enjoy oxygen therapy without taking any risks.
How Oxygen Therapy Improves Quality of Life

Besides the benefits to your breathing, oxygen therapy alters the lifestyle of living. When your blood has enough oxygen your muscles work better, then it is easier to walk, exercise and do the chores in the house without being too tired. Your mood may brighten, your sleep may become deeper and your morning headaches may disappear.
Furthermore, it is also common that a number of patients alleviate anxiety by using oxygen therapy. It is also a natural feeling to be relaxed and in control with breathing made easier. This emotion of relief is essential to the emotional health and keeps you hopeful that you can cope with pulmonary fibrosis.
Portable Oxygen for an Active Lifestyle
Previously, oxygen therapy was done at home where it would be necessary to strap oneself to a large tank. This has now completely changed with portable oxygen concentrators (POCs). These are battery-operated and portable thus you can travel, go shopping, or meet your friends without the fear of oxygen access.
The portable concentrators come with programmable settings to provide the optimal oxygen flow depending on the needs of your needs. Moreover, they can use air transportation, which gives patients an opportunity to live in a different place other than at home. Due to its flexibility, oxygen therapy is more persuasiveenient and promotes social and physical activities, which are crucial in the long-term health.
Sleep and Nighttime Oxygen Needs
Although the oxygen level may be constant in the day, pulmonary fibrosis may result in a reduction of the oxygen levels during your sleep. This happens due to slower and shallow breathing at night. Low oxygen levels at night may result in fatigue, sleeping disorders and morning headaches.
Oxygen therapy at bedtime also allows you to maintain the same level of oxygen in your body, improves the quality of your sleep, and prevents the heart and brain, which is stressful. You can also determine whether you need a supplement of oxygen at night by administering a pulse oximetry test when you are sleeping.
Traveling with Oxygen: Freedom Without Limits
Honestly, flying with a portable oxygen concentrator isn’t as dramatic as people make it out to be. Airlines and buses are usually cool with it—you just gotta jump through their hoops first. If you need to tweak your oxygen settings for that thin airplane air, definitely hit up your doc before the trip. Seriously, whoever started the rumor that oxygen therapy means you’re grounded forever… yeah, not true at all.
A little prep goes a long way. Toss all your meds in your bag, stash some extra batteries (trust me, airport outlets are a joke), and double-check with the airline that your device won’t get you side-eyed at security. With a bit of planning, you’re good to go—still living your best life, even at 30,000 feet.
The Psychological Benefits of Oxygen Therapy
Man, living with pulmonary fibrosis? It’s a lot. You’re out here gasping for air half the time, and that alone can mess with your head—feeling isolated, anxious, sometimes even straight-up depressed. Honestly, just breathing becomes this whole production.
But oxygen therapy? Total game-changer. Not saying it’s a magic fix, but it cranks the anxiety dial way down and brings back that feeling of, “Hey, maybe I can actually handle this.” People start getting their confidence back—like, actually wanting to leave the house, see friends, do normal stuff without freaking out. That boost? It’s huge. Suddenly, you’re not just surviving—you’re living again, even if it’s just in small bursts. Kind of wild how a tank and some tubing can help you grab a bit of your old self back.
Exercise and Pulmonary Rehabilitation with Oxygen
Man, when you’re struggling to breathe, moving your body feels like running a marathon underwater. The idea of exercise? Sounds like a cruel joke. But honestly, with the right folks guiding you, getting off the couch and doing some rehab can actually make your lungs and muscles less wimpy. Pulmonary rehab isn’t just some boring gym class—it’s a mix of endurance stuff, stretches, and weird breathing tricks (yes, you’ll look silly, but who cares?) to help you last longer without gasping.
And let’s not forget oxygen therapy. Basically, it keeps your O2 levels in the safe zone so you don’t end up dizzy or wiped out halfway through. It’s like a cheat code for working out—you get to push yourself without the scary side effects. Plus, the benefits? Real talk: you’ll feel braver, probably stay out of the hospital more, and just move around way easier. So yeah, it’s worth sweating through the awkwardness.
Monitoring Oxygen Levels at Home
Honestly, if you wanna know how your body’s handling oxygen therapy, just keep tabs on your oxygen levels at home. Grab a pulse oximeter—it’s that little clip thing for your finger—and boom, you’ll see your heart rate and oxygen numbers in seconds. Kinda wild how easy it is.
Now, if you keep seeing numbers under 88% or your breathing’s getting sketchier? Don’t mess around. Call your doctor ASAP. Staying on top of this stuff means you can actually do something about it—adjust meds, tweak your routine, whatever. So yeah, keeping an eye on those numbers isn’t just busywork; it’s you looking out for yourself.
Adjusting Oxygen Flow According to Needs
Honestly, how much oxygen you need isn’t set in stone—it bounces around depending on what you’re up to. If you’re jogging to catch the bus or even just walking up the stairs, your body’s screaming for more oxygen. But when you’re chilling on the couch? Not so much.
Docs usually sort out your flow rate based on tests, measuring it in liters per minute (LPM). And yeah, messing with that number on your own? Bad idea. Too little oxygen and you’ll feel like you’re climbing Everest. Too much, and that’s a whole different mess—don’t go there. Bottom line: stick to what the doc says and don’t play DIY with your oxygen settings.
Common Myths About Oxygen Use
Honestly, a lot of folks freak out about getting hooked on oxygen therapy, like it’s the gateway drug of medical treatments. Let’s be real—it’s just giving your body what it’s already craving. There’s nothing “addictive” about breathing better. Some people need it all the time, others just dip in when their O2 drops. No biggie.
And yeah, people love to act like oxygen tanks are ticking time bombs. Not true—unless you’re planning on juggling them next to a bonfire or something. Modern systems are super safe if you don’t do anything wild. Bottom line: if you actually know what you’re doing, there’s nothing to be scared of. Get the facts, breathe easy.
Cost and Insurance Coverage for Oxygen Therapy
Oxygen therapy isn’t exactly cheap—especially if you need it all the time. But hey, if your doctor says you really need it, most insurance plans or national health systems will pick up the tab (or at least most of it). Still, it’s a smart move to chat with your doctor about any government help, supplier deals, or ways to get some financial relief. Some companies actually have rental plans or assistance programs to make things a little less brutal on your wallet. Don’t be shy about asking; people do it all the time.
Living Positively with Pulmonary Fibrosis
Yeah, getting hit with a pulmonary fibrosis diagnosis? That’s a punch to the gut, no sugarcoating it. But look, it doesn’t mean you’ve gotta lock yourself away or wave goodbye to good times. Oxygen therapy’s actually a total game-changer—lets you keep moving, breathe without feeling like you just ran a marathon, and, most importantly, hang out with your favorite people without feeling wiped out.
And honestly, it’s not just about the oxygen tanks and tubes. There’s a whole toolkit out there: eating decent food (most days, at least), chatting with folks in the same boat, maybe even letting a therapist help you untangle some of the mental junk. You focus on what you can actually do, make those breaths count, and don’t sweat the stuff that’s outta your hands. That’s the secret sauce.
The Future of Oxygen Therapy and Pulmonary Care
You know, it’s honestly wild how fast this stuff moves. Medical tech isn’t just creeping forward—it’s sprinting. Now you’ve got these wearable gadgets tracking your oxygen 24/7, kinda like a Fitbit but for your lungs. And those old-school, clunky oxygen machines? Forget it. The new ones are tiny, barely make a sound, and actually do their job without making you feel like you’re lugging around an engine.
There’s even talk about some wild regenerative therapies—like, scientists are actually poking around trying to figure out how to undo lung scarring. Sounds sci-fi, but hey, who knows?
For now though, oxygen therapy is still the MVP. It’s reliable, gets the job done, and helps people with pulmonary fibrosis actually enjoy life instead of just surviving. Stick with your checkups, use the new tech, and you’ll probably end up living longer and feeling a heck of a lot better. Not a bad deal, honestly.

Conclusion: Oxygen Therapy—Your Breath of Hope
Look, with pulmonary fibrosis, the aim isn’t just to scrape by—it’s about actually living your life, not just counting the days. Getting enough oxygen? That’s a game-changer. Your heart gets a break, you don’t feel like you’re gasping for air 24/7, and you start to feel like you’ve got some say in how things go.
Oxygen therapy isn’t some magic fix, but when you stack it up with meds, moving your body (even if it’s just a walk to the mailbox), and having folks around who get it? Suddenly, the walls don’t feel so close in.
Honestly, every single breath counts. And yeah, the right oxygen plan can make it so much less of a struggle. Feels less like you’re just surviving and more like you’re actually here.
