TB Effusion vs Pulmonary TB – Understanding the Difference, Symptoms, and Care
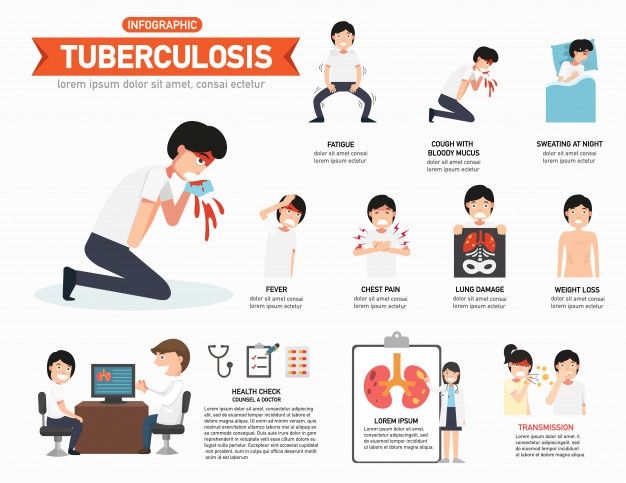
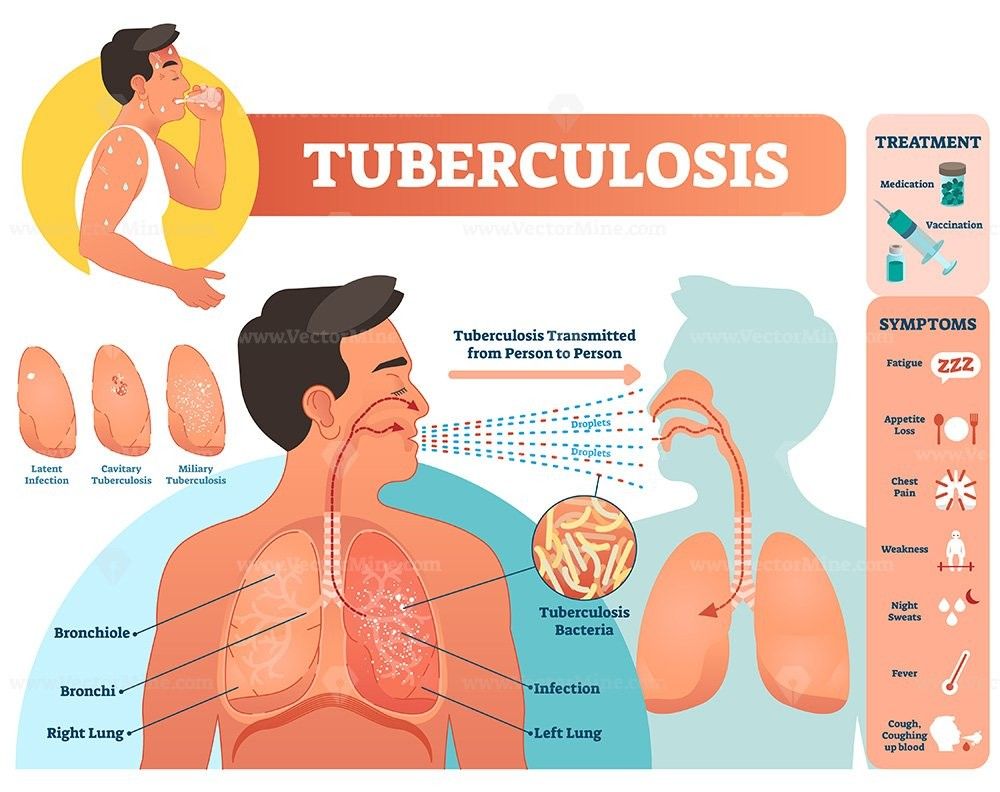
Tuberculosis (TB) is the infectious disease that is caused by Mycobacterium tuberculosis, one of the oldest infectious diseases in the world. Even though TB may attack other body organs, most people only consider lung infections. Tuberculous Pleural Effusion (TB Effusion) and Pulmonary TB are the two common types of tuberculosis which may confuse a person.
Although they are all caused by the same bacteria, they are widely differentiated with respect to their sites of infections, their symptoms, diagnosis and treatment.
An extensive and detailed two column comparison that clarifies such variances in details to the advantage of the patient is given below.
TB Effusion (Tuberculous Pleural Effusion)
Definition |
Cause |
Pathophysiology bacteria, which makes confirmation in the lab difficult. |
|
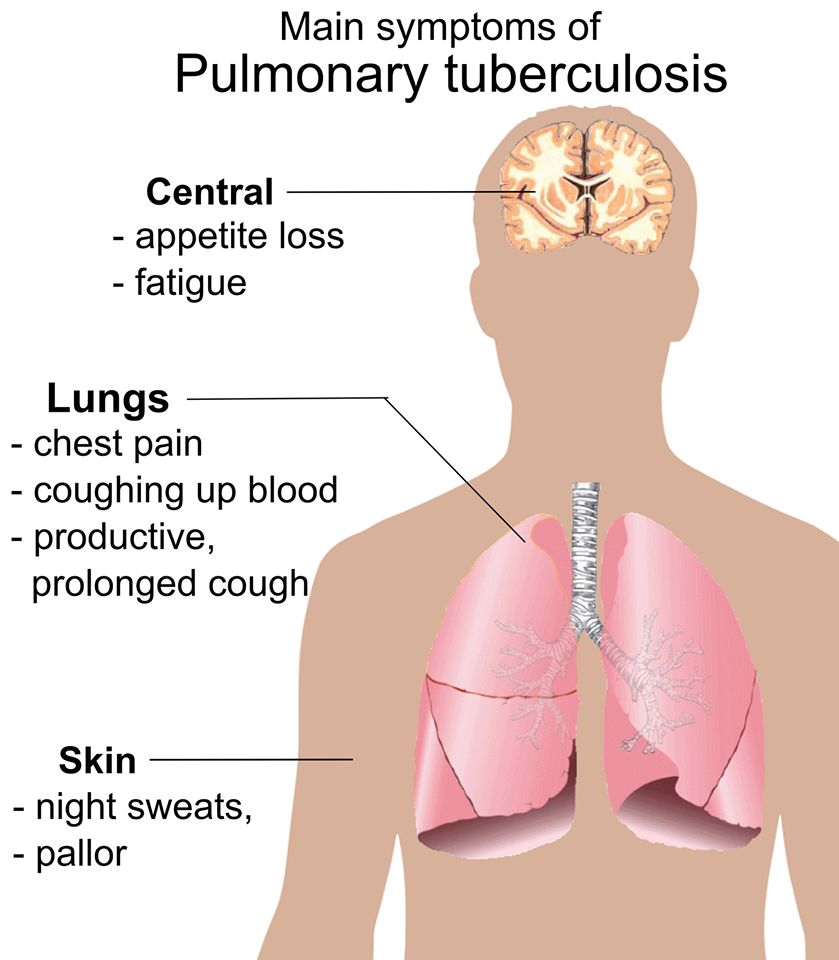
Common Symptoms • A chronic dry cough. • Fluid pressure-induced breathlessness. |
Physical Findings |
Contagiousness |
Diagnosis: • Pleural fluid analysis: high ADA (adenosine deaminase), high protein, and lymphocyte dominance. • Thoracoscopic pleural biopsy if the diagnosis remains unclear. |
Radiological Appearance • The opacification of one side of the chest is homogenous. • Mild pulmonary collapse or mediastinal deviation may occasionally occur. |
Laboratory Findings • The cause of TB is confirmed by ADA levels of more than 40 U/L. • In most cases, bacteria cannot be seen on the smears. |
Treatment • In severe cases, prolonged therapy (nine to twelve months). • Drainage of pleural effusion when there is a large effusion, causing distress to the patient. • Corticosteroids may be used to reduce inflammation and hasten healing. |
Complications • Chronic empyema (pus collection) and recurrence. |
Prognosis |
Prevention |
|
Dietary Advice • Proteins e.g., milk, eggs, fish, pulses. • Drink much water to help your lungs work. |
Follow-up |
vs
Pulmonary TB (Tuberculosis of the Lungs)
Definition |
Cause |
Pathophysiology When the bacteria enter the lungs, the immune system forms granulomas to prevent their entry. These granulomas break up when the immune system is compromised and this leaves live bacteria that spread and destroys lung. tissue. The openings that are a result of this process appear on X-rays. |
|
Common Symptoms • Cough up blood or bloody flem. • Gripping pains and chest aches. • Weight loss and decreased appetite. |
Physical Findings • Lung consolidation symptoms. • Cavitary images are present. |
Contagiousness |
Diagnosis The presence of bacterial DNA is confirmed by GeneXpert or PCR test. • A chest X-ray shows the existence of cavities, nodules, or infiltrates. • The IgG test for interferon-gamma or the tuberculin skin test (TST). |
Radiological Appearance • Risk factors for such large and infectious TB lesions include chronic cavitary fibroses in the upper lung. |
Laboratory Findings |
Treatment • In cases of extensive pulmonary damage, oxygen treatment. • Prolonged treatment for MDR-TB, or multidrug-resistant tuberculosis. |
Complications • Proliferate to other organs (TB meningitis, military TB). • If therapy is not completed, then multi-drug resistance may develop. |
Prognosis |
Prevention • Avoid contact with infectious • Use of masks and adequate ventilation in crowded places. |
Dietary Advice • Avoid cigarettes and prepared foods. • Get enough sleep and take water enough. |
Follow-up • Continued observation for relapse. |
Key Comparison Summary
Site of Infection: Pulmonary TB occurs in tissue of the lungs whereas TB diffusion occurs in the pleural space.
- Transmission: Pulmonary TB is contagious but TB diffusion is not.
- Major Symptom: TB Effusion presents as dyspnea and chest pain, whereas the pulmonary TB presents as a persistent cough and sputum.
Diagnosis Sputum testing is required in pulmonary TB, and pleural fluid testing is required in TB diffusion.
Treatment: Supportive management, however, is the same but they all need the basic anti-TB medicines.
Conclusion - Two Faces of the same disease
Despite the fact that TB Effusion and Pulmonary TB are caused by Mycobacterium tuberculosis, the physiological effects of the two are hugely different. Although TB is an active infection in the lungs, which may be transmitted to other individuals, the diffusion of TB is due to an infection or immune response in the pleural cavity.
In spite of their differences, both types can be treated properly and on time. Taking prescriptions, eating well and avoiding alcohol and tobacco.
a vital role in recovery.
It is also very paramount to protect others, in regards to pulmonary tuberculosis; patients should wear a mask, observe good hygiene and follow the instructions of their doctors keenly.
Seek medical attention immediately in case of persistent cough, chest pains, and unexplainable fever. TB is treatable; early medical care, adherence to treatment and good awareness of the public health is essential.
