IHD vs LVF – Understanding the Difference, Symptoms, and How to Protect Your Heart
Heart disease is one of the leading causes of death in the globe. Among the most dangerous and the most closely related heart diseases, there are Ischemic Heart Disease (IHD) and Left Ventricular Failure (LVF). In spite of the fact they are caused differently, have various symptoms, and are treated differently, both may influence the ability of the heart to beat properly.
Prevention, early diagnosis and effective management of these conditions is the first step towards gaining an insight into the same. We are going to discuss the meaning of IHD and LVF, the difference between them, and the manner in which their adverse effects can be prevented.
What Is Ischemic Heart Disease (IHD)?
The build up of the plaque results in the narrowing or blockage of the arteries that deliver blood to the heart resulting in the Ischemic Heart Disease (IHD) or Coronary Artery Disease (CAD). This complicates the ability of the heart to perform its work by reducing blood flow which is rich in oxygen to the heart muscle.
The most common cause of IHD is called atherosclerosis, which is a disorder, where fatty deposits, cholesterol, and other substances accumulate to create a thick lining of the inside of the arteries. This build-up ultimately hinders the circulation of blood leading to angina, dyspnea or a heart attack.
Many years later, IHD occurs gradually, and often does not produce any symptoms until a blockage becomes extremely severe.
What Is LVF (Left Ventricular Failure)?
Left ventricular failure (LVF) is a form of heart failure that occurs when the heart cannot pump blood properly to the rest of the body organs because of the failure of the left ventricle (the main chambers of the heart).
This causes blood to stagnate in the lungs and fills the lungs with fluid thus making breathing a challenge.
Acute LVF may occur suddenly whereas chronic LVF develops over time.
LVF is often caused by IHD, hypertension, heart valve disorders or previous heart attacks.
The body fails to receive sufficient oxygenated blood, and this leads to fatigue, lightheadedness and swelling when the left ventricle becomes weak.

IHD vs LVF – The Key Difference
IHD and LVF differ in spite of their associations.
A complication with the blood flow to the heart muscle is known as IHD.
An issue of the pumping of the heart is known as LVF.
In other words, the LVF can be the result, and IHD the cause.
LVF can occur subsequently when the blood supply of the heart is terminated in prolonged periods (as in IHD) thus weakening or injuring the heart muscle.
Therefore, untreated, IHD can later develop into LVF.
Feature Left Ventricular Failure (LVF) Ischemic Heart Disease (IHD)
Definition Reduced blood flow to the heart Weakness of the left ventricle that
muscle because of narrowed arteries decreases the pumping power.
Primary Cause Atherosclerosis (plaque deposition) IHD, hypertension, or valve disease.
Main Symptom Pain in the chest (angina) dyspnea, weakness,retention of fluids.
Onset Gradual May be either gradual or sudden.
Focus Tissue Improving blood flow Strengthening heart function.
Risk of Progression Risk may result in LVF Can result in complete heartfailure.
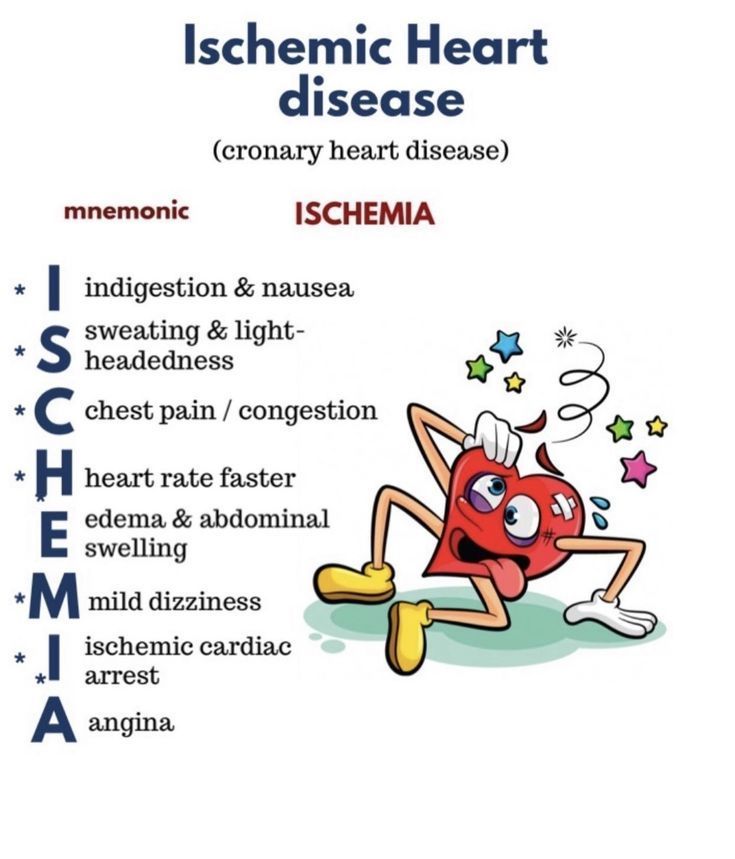
Symptoms of IHD
- Early detection of the symptoms of IHD prevents severe damage of the heart.
- Breathlessness
- Neck, jaw, shoulder, or arm pain
- Weakness and exhaustion
- Exerting oneself causes one to sweat or feel nauseated.
IHD may often be silent, that is, it does not present any symptoms until such a severe event as a heart attack occurs. Checkups are thus a very important thing to do especially when you are at risk such as having high cholesterol, obese or smoking.
Symptoms of LVF
When the left ventricle is not pumping the blood properly, a number of warning signs appear, and they include:
- Fatigue and difficulty in undertaking daily tasks.
- Edema caused by the retention of fluid in the legs, ankles and abdomen.
- An erratic or fast heartbeat
The acute pulmonary edema, or pulmonary edema that fills the lungs and requires an emergency treatment, may emerge quickly because the sudden weight increase due to the presence of fluid in the LVF leads to pulmonary edema.
Causes and Risk Factors
Causes of IHD
- The plaque that is deposited in the arteries is called atherosclerosis.
- Increased amounts of triglycerides and cholesterol.
- The long-term pollutants and smoking.
- Diabetes and out of control obesity.
- Lack of physical exercises and unhealthy lifestyle.

Causes of LVF
- Hypertension or high blood pressure, which causes an unreasonable strain on the heart.
- Defects in the heart valves
- Abuse of drugs or alcohol
- Anemia or chronic pulmonary disease.
How Doctors Diagnose IHD and LVF
Diagnosis of IHD
Doctors use a variety of tests in order to diagnose IHD:
- Electrocardiogram (ECG) is an examination of irregular heartbeats.
- Echocardiogram (ECHO) is a test that measures the cardiac performance through the application of sound waves.
- Stress Test: This is a test that checks the performance of your heart during exercise.
- Blood tests are used to measure cardiac enzymes that increase the level when a heart attack takes place.
Diagnosis of LVF
Doctors can:
- The ejection fraction (EF), or amount of blood that the left ventricle expels is measured through Echocardiography.
- An MRI or a CT scan is able to generate an image of the heart in small grains.
- The BNP test of blood reports the level of heart failure.
Treatment Approaches
Treatment for IHD
The two main objectives of the treatment of IHD are the restoration of the blood flow and the blockages.
- Aspirin, beta-blockers, nitrates, and statins are medications that lower cholesterol and blood circulation.
- Blockages in arteries can be opened with the help of an angioplasty and stenting.
- Incorporation Coronary artery bypass surgery involves the establishment of a new pathway in which blood circulates to the heart muscle.
- Lifestyle management is diet, exercise and smoking cessation.
Treatment for LVF
The major goal of the LVF treatment is to treat the weakening heart.
- Beta-blockers, ACE-inhibitors, and aldosterone antagonists, and diuretics are used to eliminate the excess fluid.
- Pacemakers and defibrillators are implantable devices that are employed to control the heartbeat.
- Surgery: replacement or repair of valves, in the worst case scenario, heart transplantation.
- Rehabilitation entails physical exercises to strengthen the heart and change of lifestyle..
Diet and Lifestyle – What to Avoid and What to Follow
The lifestyle decisions are critical to your recovery and prevention despite IHD or LVF.
Foods to Avoid:
- Salt retention can be brought about by excess salt.
- Desserts and sweet drinks.
- Processed or red meats
- Caffeine and alcohol (in excess)
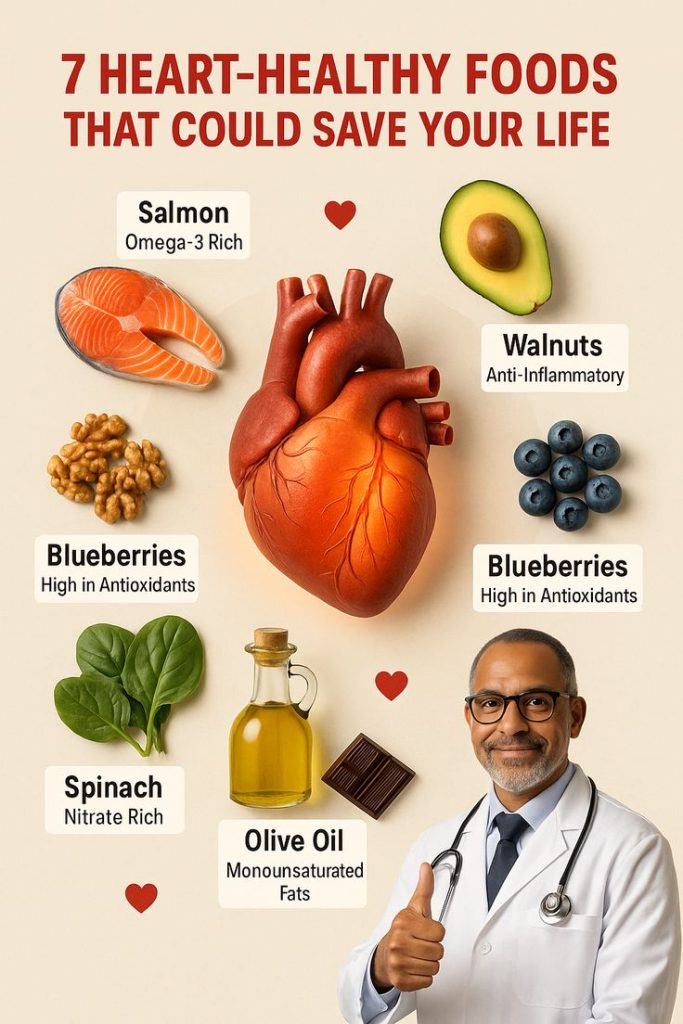
Healthy Foods to Include:
- Fresh produce and fruits
- Legumes and whole grains
- Lean (chicken with no skin, fish) proteins.
- Nuts and olive oil
- A lot of water
Daily Habits to Follow:
- Moderate exercise (30 minutes yoga or walking per day)
- Instantly stop smoking
- Regulation of cholesterol and blood sugar.
- Meditation or breathing exercises to deal with stress.
- 7–8 hours of sleep each day
Emotional and Mental Health in Heart Patients
Heart conditions affect both your emotional well-being and physical one.
Anxiety, fear and depression are often found in patients with IHD or LVF especially after they leave hospital.
Becoming a member of heart support groups, discussing with your doctor and being positive can all make a great difference.
It will be remembered that mind strength and regular lifestyle are equally beneficial in the healing of the heart as medicine.

When to See a Doctor
The chest pain should be severe and sudden; in this case, it is necessary to seek medical attention immediately.
- Shortness of breath or unconsciousness.
- The edema or abrupt weight gain.
- Lightheadedness or palpitations.
Early diagnosis saves life. A minor problem with the heart may become a fatal failure in case it is not given the treatment at the right time.

Prevention – The Best Protection
LVF, as well as IHD, can be prevented by healthy living.
Start simple changes: start eating better, exercise more, quit cigarette smoking, and monitor cholesterol and blood pressure.
Your doctor recommends regular heart screening, especially in case of having a family history of heart conditions.
Prevention is a routine that will help you reduce the risks of both IHD and LVF and extend the lifespan of your heart.
Conclusion – One Heart, Many Reasons to Protect It
LVF and IHD go hand in hand and one handicaps the role of the heart pumping blood, the other is the handicap of blood supply to the heart.
The keys of prevention are the awareness of the difference, detecting early symptoms, and living a heart-healthy lifestyle.
In case you have been diagnosed of heart disease, you still can have a normal and active life and with immediate treatment, self responsibility and medical advice.
It beats your heart a second, and thou art a care of it.
